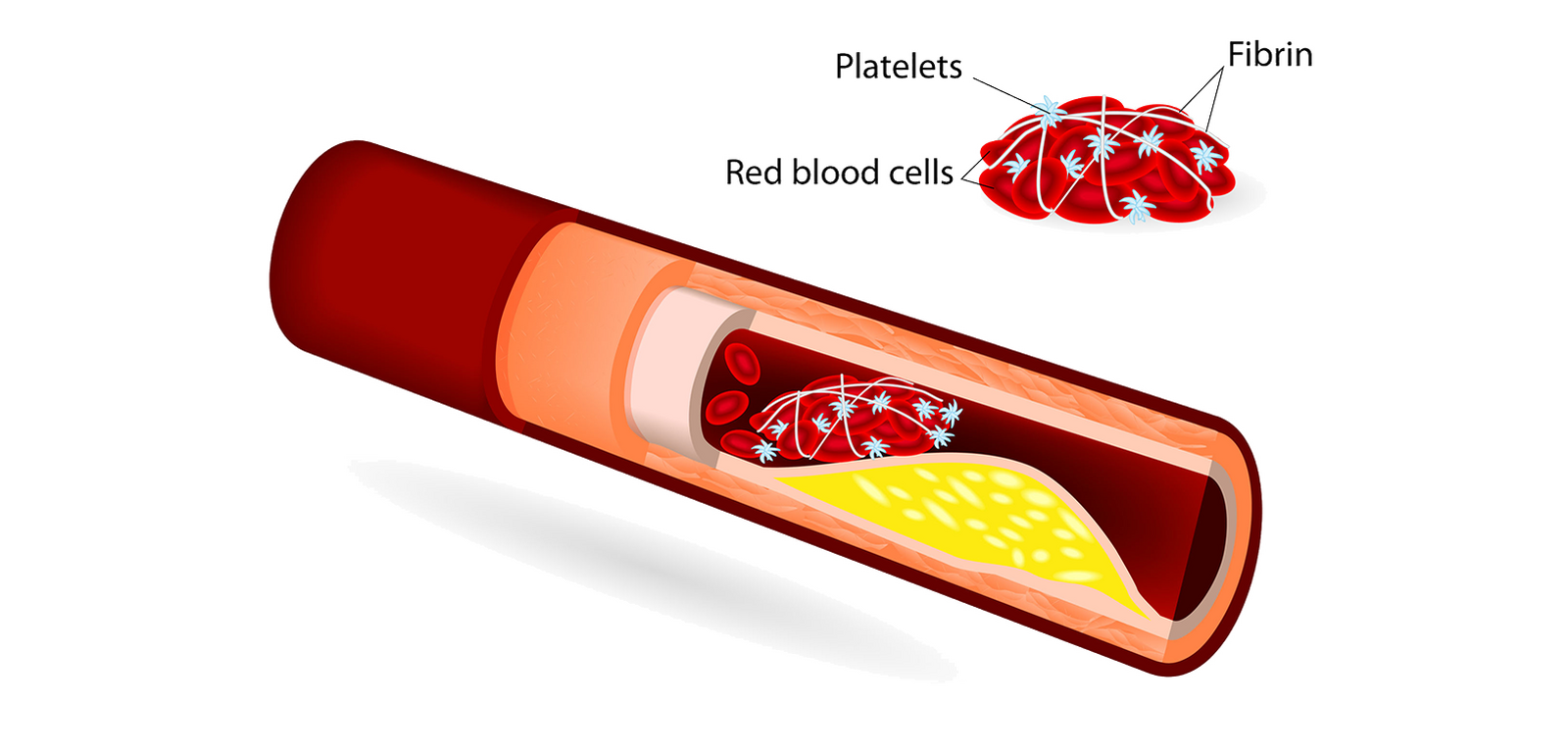
Blood is never just liquid. It carries information, defense, memory. It responds fast to damage. When there’s injury, clotting kicks in to plug the leak. That’s how we survive. But the same process, when misfired, can harm. Clots that form without injury, or that don’t dissolve, block flow. They turn protective instinct into danger. The body doesn’t always know when to stop sealing. And that’s where the trouble begins.
Clots can travel and lodge where they shouldn’t
A clot in the leg might not stay in the leg. It can move. When it does, it rides through vessels, looking for a tighter space. The lungs are a common landing point. So is the brain. When that happens, tissue suffers. Oxygen cuts off. Symptoms don’t always wait—they crash in. And once flow is blocked, cells start dying. That’s why time matters, not just diagnosis.
Some people never feel them forming
Clots don’t always announce themselves. They don’t knock or warn. Sometimes the first sign is pain. Other times it’s breathlessness, out of nowhere. But often, there’s no sign at all. Until one morning, the leg swells. Or walking becomes strange. Or a cough becomes sharp. By then, it’s moved past prevention. Quiet threats are harder to track, especially when they wear no uniform.
Long flights and long recoveries share a common enemy
Stillness. It may sound restful, but it isn’t always safe. On planes, blood pools in the legs. In hospitals, patients lie in bed, unmoving. Both conditions slow flow. Slowed blood is sticky blood. It starts gathering, building, nesting. A clot doesn’t need much space to grow. Long periods of immobility let it do just that. And sometimes, what begins during sleep ends in emergency.
Hormones shift clotting behavior in invisible ways
Estrogen changes things. It thickens the blood. Birth control pills and pregnancy both increase clot risk. So does hormone therapy. These shifts are natural, but not without price. Some people carry hidden mutations, like Factor V Leiden. On their own, they’re silent. Paired with hormonal changes, they ignite. That’s why some clots surprise the young, not the elderly. Blood carries secrets, and sometimes they surface suddenly.
Cancer doesn’t just attack organs—it also hijacks blood
Malignancy alters the body’s entire rhythm. Tumors send signals that confuse clotting. The blood becomes hyperactive, clotting even without injury. Chemotherapy worsens this. So do central lines and ports. Clots in cancer patients don’t always follow patterns. They appear in strange places, with strange timing. Often, before the cancer is even diagnosed. That’s one reason routine checks matter. The clot is sometimes the first messenger.
Smoking shrinks vessels and hardens circulation
Each cigarette constricts. Not just lungs, but blood vessels. Smoking damages the lining of the veins. It makes blood more prone to clot. Platelets become aggressive. Clots find easier homes in narrowed spaces. It’s not just long-term smokers at risk. Occasional use still shifts the chemistry. In those with other factors, it’s often the tipping point. Blood remembers what the lungs breathe.
When the legs ache and swell, something deeper may be stirring
A deep vein thrombosis doesn’t always roar. Sometimes, it pulses quietly behind the calf. The skin feels hot. Movement brings a dull throb. Or maybe nothing feels off until walking changes. DVT hides behind normal soreness. But the stakes are high. If it breaks loose, the lungs are its next stop. A pulmonary embolism doesn’t wait for permission—it crashes through.
The clot that blocks a brain artery is a thief of time
Strokes are not slow. They come with confusion, drooping, slurred words. Sometimes all at once. When a clot hits the brain, minutes count. Every lost second means dying neurons. Not every stroke is from a clot—but many are. Atrial fibrillation, an irregular rhythm, lets blood pool in the heart. From there, a clot can shoot up to the brain. That’s how one misfired heartbeat becomes a life split in two.
Heat and dehydration make blood sluggish and sticky
Summer isn’t always friendly to blood flow. When water runs low, blood thickens. High heat pulls moisture from the body. The result is slower circulation, especially in veins. In people prone to clotting, this triggers trouble. It’s not just deserts and saunas—it’s long days without enough water. The body keeps trying to cool down, while the blood keeps warming up. A dangerous mismatch.
Compression gear can help—but not without movement
Socks and sleeves push blood upward, back toward the heart. They help when movement is limited. But gear alone isn’t enough. Blood needs muscle movement to stay mobile. Calf pumps. Foot flexes. Even standing counts. Without that, compression becomes decoration. Prevention needs partnership—mechanical and biological working together. Otherwise, the clot waits for its chance.
Flights over four hours start the risk window
Economy class syndrome isn’t just a phrase. After four hours, risk begins climbing. Not for everyone, but enough to notice. Small movements help: ankle rolls, short walks, hydration. Some wear compression socks. Others avoid alcohol. Flying itself isn’t dangerous—but flying still is. The cabin dries you out. The seat limits motion. The blood adapts, sometimes in the wrong way.
Trauma turns clotting into overdrive
Broken bones, bruises, surgeries—each awakens the clotting system. It’s not malfunction, it’s survival. But the system can overdo it. After trauma, blood becomes hyper-alert. Clots form to protect—but then they stay. Some lodge in lungs. Others form in healing limbs. The body saves itself and, in doing so, sometimes risks itself. That’s why trauma patients are closely watched for clots, even weeks after the injury.
Obesity adds pressure and slows blood return
Fat doesn’t just sit on the surface. It presses on veins, especially in the abdomen. That pressure slows the return of blood to the heart. The legs carry the burden. Slower blood means greater clot risk. Add in less activity, more inflammation, and hormonal shifts—risk multiplies. Clots don’t need visible damage. They need conditions. Obesity provides several, all at once.
Blood thinners don’t dissolve clots—but they prevent more
Anticoagulants stop growth. They don’t undo the clot already formed. But they matter. By thinning the blood, they reduce chance of new clots forming. And they give the body time to break down what’s already there. They require balance. Too little, and risk remains. Too much, and bleeding follows. The right dose saves lives. But it needs watching, always.
Some people inherit risk without knowing
Clotting disorders run quietly in families. Protein C deficiency. Antithrombin problems. Factor V Leiden. Often, people find out after a clot. Or during pregnancy. Or before surgery. Routine tests don’t always include these. But family history tells a story. A cousin with early stroke. A sibling with leg clots. Genetics don’t guarantee clots—but they change the map. And knowing the terrain helps you walk it safer.
Aspirin helps in some cases, not all
Aspirin thins platelets, not the entire blood. It helps in arterial clots. Less in veins. For stroke prevention in high-risk people, it’s standard. But for DVT, it’s not enough. Still, people self-medicate, thinking it’s protection. But clot types differ. And so do treatments. What helps in one place may hurt in another. That’s why guessing doesn’t work here. Neither does general advice.
Diet shifts clot risk quietly and slowly
Foods affect clotting in indirect ways. Leafy greens raise vitamin K, which strengthens clotting. Garlic, turmeric, and ginger thin the blood slightly. High-fat meals, sugar, and dehydration make clots more likely. Processed foods play a subtle role. Salt retains water. Add inflammation, and the stage is set. Food won’t create clots alone. But it can push the chemistry. Enough to tip the balance.